What is an aortic aneurysm?
The aorta is the main artery that carries oxygen-rich blood from the heart to the rest of the body. An aortic aneurysm can occur when a part of the aorta becomes weak, bulges out and forms a balloon-like enlargement.
Types of aortic aneurysm
There are two main types of aortic aneurysm; a thoracic aortic aneurysm (TAA) and an abdominal aortic aneurysm (AAA). A TAA is a bulge or enlargement of the aorta located in the chest area. An AAA is a bulge or enlargement in the aorta in the abdominal area.
Within thoracic aortic aneurysms, there are further sub-types; ascending, descending and arch. An ascending aortic aneurysm occurs in the part of the aorta that extends upwards from the heart. A descending aortic aneurysm occurs in the section of the aorta which is located in the lower part of the chest, extending downwards towards the abdomen. An aortic arch aneurysm forms in the curved upper section of the aorta and can affect the vital blood vessels which supply blood to your head and neck.
An aortic aneurysm can be a life-threatening condition as it can rupture and cause internal bleeding. If this happens, mortality can be as high as 54% at six hours after onset or 76% at 24 hours, and emergency treatment in the form of surgery is required.
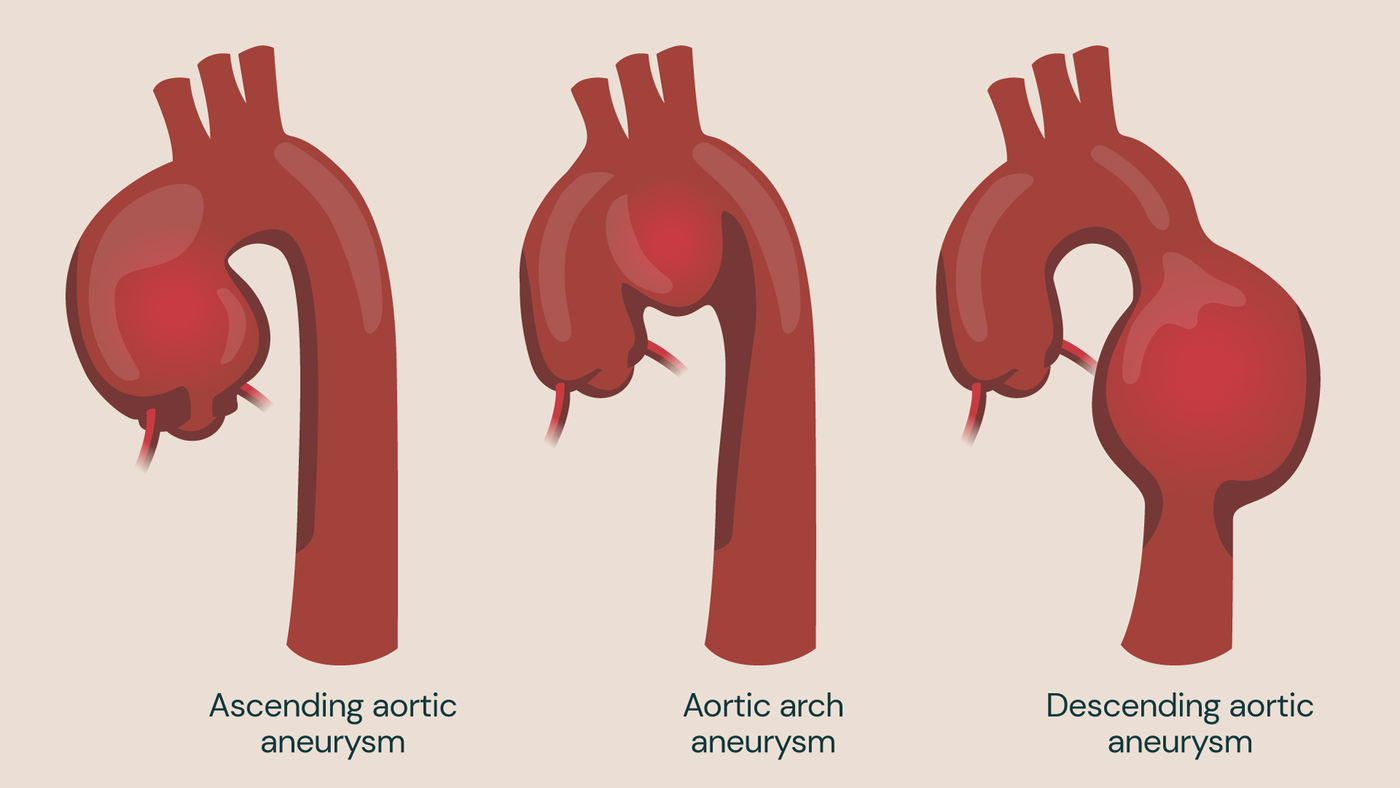
Thoracic aortic aneurysm (TAA)
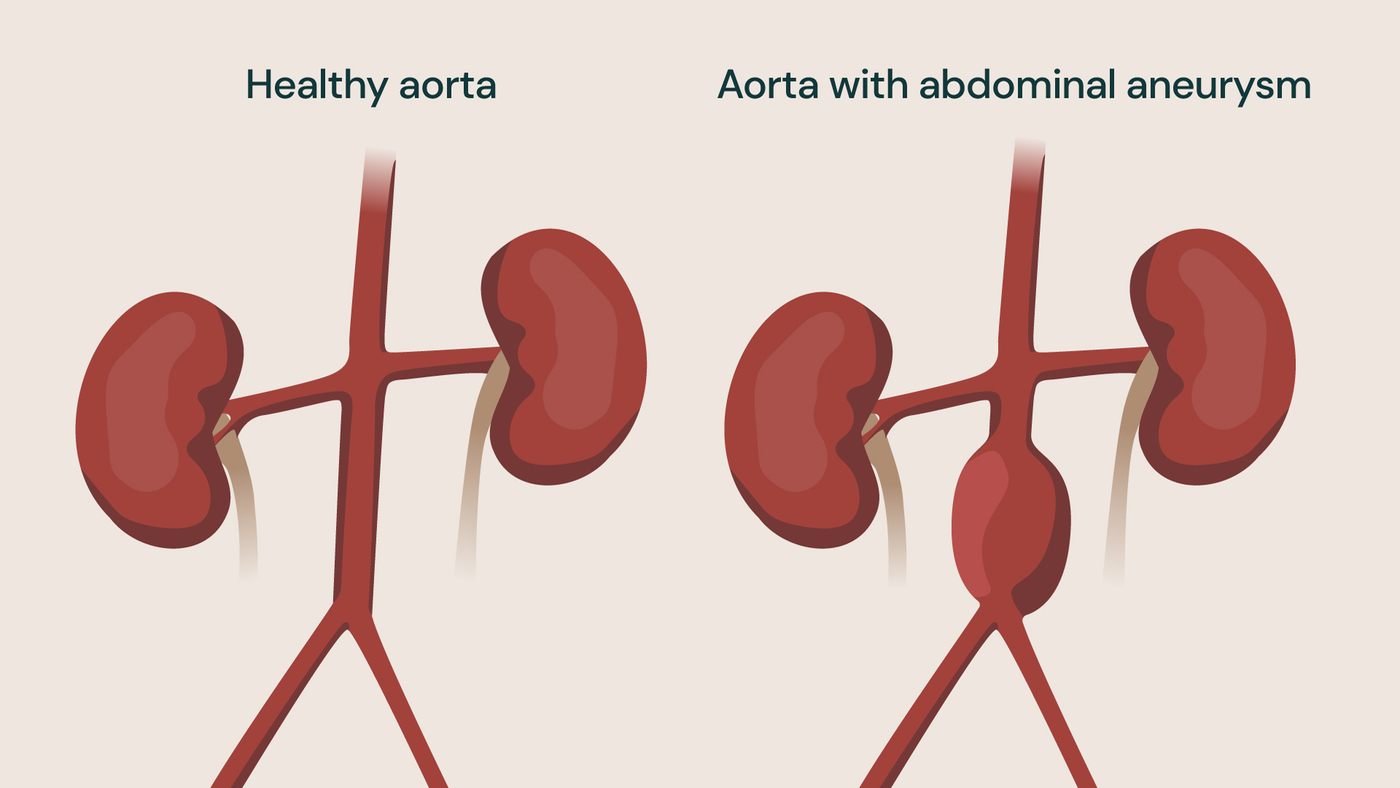
Abdominal aortic aneurysm
Aortic aneurysm symptoms
In many cases, aortic aneurysms do not cause any symptoms, especially when they are small. Aneurysms typically grow 1-2mm per year, so it may be several years before you feel any discomfort caused by an aneurysm. The typical threshold for operating on an aortic aneurysm is a diameter of 5.5cm in men and 5cm in women.
When the aneurysm grows larger, it can cause symptoms such as:
- pain in the chest or back
- abdominal pain or discomfort
- shortness of breath
- difficulty swallowing
- hoarseness
Aortic aneurysms can be life-threatening if left untreated. Early detection and management can help prevent complications and improve outcomes for patients.
If you have been diagnosed with an aortic aneurysm, you will be invited for regular appointments to monitor its growth and assess when the best time is to intervene with surgery.
If you experience any symptoms associated with an aortic aneurysm, it is important to seek medical advice quickly. However, several of the above symptoms overlap with other conditions such as aortic dissection or aortic ulcers, so a scan may be necessary to determine the cause of your symptoms.
What causes aortic aneurysm?
There are several risk factors that can cause the weakening of the aortic wall, leading to an aortic aneurysm.
Age: As people get older, the aortic wall can weaken, making it more susceptible to aneurysms. Patients aged 65 and over are most likely to experience an aneurysm, with the risk increasing by 4% every 10 years.
Gender: Men are more likely to experience an aortic aneurysm than women, although women are more likely to experience a rupture.
Smoking: Smoking damages the walls of the blood vessels and increases the risk of developing an aortic aneurysm.
High blood pressure: Increased pressure in the blood vessels can put a strain on the aortic wall, resulting in an aneurysm.
High cholesterol: Cholesterol is a fatty substance in your blood which can build up in your arteries and increase your risk of aortic aneurysms.
Family history: Up to half of all thoracic aortic aneurysms are inherited and your risk level can be determined with genetic testing.
Connective tissue disorders: Certain genetic conditions such as Marfan syndrome and Ehlers-Danlos syndrome can cause weakness in the aortic wall. This makes an aneurysm more likely.
Complications of aortic aneurysms
Aortic aneurysms can have several complications if left untreated.
Rupture: One of the most serious complications of aortic aneurysms is rupture. If the aneurysm ruptures, it can lead to massive internal bleeding, which can be life-threatening.
Aortic dissection: An aortic dissection occurs when there is a tear in the inner layer of the aortic wall. This can cause blood to flow between the layers and separate them. This can lead to reduced blood flow to vital organs and can also be life-threatening.
Embolisation: Small pieces of blood clots or plaque can break off from the aneurysm and travel to other parts of the body. In some cases, this causes a blockage in blood vessels and leads to organ damage.
Peripheral artery disease: Some aneurysms are located in the abdominal aorta. These can compress the blood vessels that supply blood to the legs, leading to peripheral artery disease.
Aortic valve regurgitation: In some cases, an aortic aneurysm can cause the aortic valve to stop working properly. This leads to aortic valve regurgitation where the blood flows back into the heart, instead of out to the rest of the body.
Organ damage: Large aortic aneurysms can compress adjacent organs such as the kidneys, liver, or spleen. This can result in organ damage and dysfunction.
Limb ischemia: An aortic aneurysm can compress the blood vessels that supply blood to the limbs. This can lead to reduced blood flow and ischemia (lack of oxygen) to the limbs.
Aneurysm growth: Aortic aneurysms can grow in size over time, typically by up to 2mm per year, which can increase the risk of rupture or dissection.
Infection: Aortic aneurysms can also become infected, which can lead to serious complications such as sepsis and organ failure.
Blood clots: Aortic aneurysms can promote the formation of blood clots, which can lead to pulmonary embolism, stroke, or heart attack.
It is important to note that not all aortic aneurysms will lead to these complications. If you have been diagnosed with an aortic aneurysm, you should speak to your consultant about how to manage the condition. This will also help to prevent potential complications.
Preventing aortic aneurysms
Some risk factors for aortic aneurysms such as age and genetic conditions cannot be prevented. However, there are certain lifestyle changes that can reduce the risk of developing the condition. These include:
- quitting smoking
- maintaining a healthy weight
- exercising regularly
- managing high blood pressure and cholesterol levels
Diagnosing aortic aneurysms
Aortic aneurysms are often detected during routine medical examinations or imaging tests including:
- chest X-rays
- CT scans
- cardiac MRI scans
If an aneurysm is suspected, further tests may be carried out, such as an ultrasound or angiography. This will determine the size and location of the aneurysm, which will inform treatment options. These tests may also be carried out if the other tests haven’t provided enough information about the aneurysm.
50% of cases of aortic aneurysm are thought to be inherited, so we recommend genetic testing if a close relative has experienced an aortic aneurysm. Learn more about our specialist private genetic testing service which can help to determine your risk of aortic disease.
Aortic aneurysms treatment
The treatment of aortic aneurysms depends on the size and location of the aneurysm. It also depends on the overall health and age of the patient.
Small aneurysms may be monitored regularly to check for any growth, while larger aneurysms may require surgery. It’s also important to weigh up the risk of rupture against the risk of potential complications from surgery.
When an aneurysm is less than 6cm in diameter, treatment is not always recommended. A TAA of 5.5cm has a rupture risk of 5% per year and therefore, when other factors about the patient’s age and health are taken into consideration, a ‘do nothing’ approach may be chosen.
However, a patient with a 6.5cm aneurysm has a 10% risk of rupture each year, and therefore is more likely to be referred for aortic repair surgery. The risk of rupture increases in line with the size of the aneurysm, and aneurysms typically grow 1-2mm per year.
Surgical options can repair or replace the damaged section of the aorta. In some cases, medications may be prescribed to lower blood pressure and reduce the risk of aneurysm rupture.
Minimally invasive surgery
Minimally invasive Thoracic EndoVascular Aortic Repair (TEVAR) is now the recommended procedure for aortic repair, as an alternative to open surgery.
This involves inserting a catheter into the blood vessel through a small incision in the groin. A stent graft is then guided to the site of the aneurysm. The stent graft reinforces the weakened area of the aorta and reduces the risk of rupture.
Endovascular repair is less invasive than open surgery and has a shorter recovery time. The mortality rates associated with TEVAR are significantly lower than those for open repair surgery, with a significant survival benefit persisting for nine years after TEVAR surgery, when compared to open repair surgery.
TEVAR may not be suitable for all types of aneurysms and could require additional procedures or monitoring. However, TEVAR is thought to be especially suitable for older patients who may struggle with the recovery associated with open surgery, instead benefiting more from small incision surgery.
Your consultant will work with you to determine the most appropriate surgical option based on your specific condition.
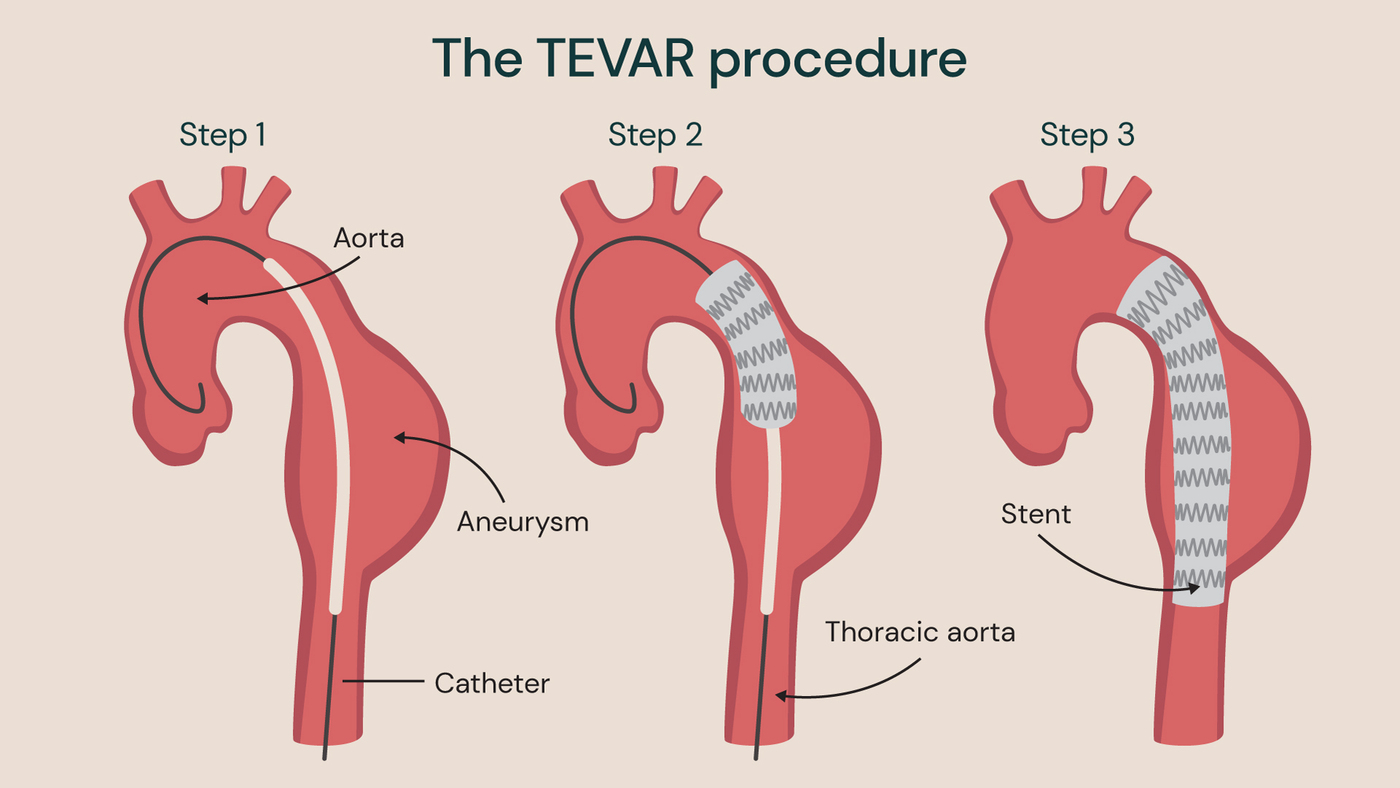
An example TEVAR procedure with a stent in place to treat a descending aortic aneurysm.
Open chest surgery
Another option for the treatment of aortic aneurysms is open thoracic aortic aneurysm repair surgery. This involves making a large incision in the chest or abdomen to access the aneurysm. The surgeon then replaces the damaged section of the aorta with a synthetic graft. This procedure is highly effective and durable, but it also carries significant risks, such as bleeding, infection, and organ damage.
An ascending aortic aneurysm may extend to the aortic valve, called an aortic root aneurysm. This can damage the valve, meaning that your surgeon may need to replace it with a prosthetic valve, along with the damaged section of the aorta.
This carries additional surgical risks and if a mechanical aortic valve is used, you will need to take blood thinning medication for life to avoid blood clots. As prosthetic valves need replacing over time, you may require surgery again in future.
If you have an aortic root aneurysm and your aortic valve is still healthy, the David Procedure may be of benefit. It involves removing the damaged, weakened section of the aorta and replacing it with an artificial tube graft. The graft is then attached to the healthy aortic valve and blood vessels.
As the stretching pressure of the aneurysm is removed from the healthy aortic valve following surgery, it can return to its normal function. The David Procedure allows for preservation of the patient’s own aortic valve, which can avoid reliance of long-term blood thinning medication.
If you have an aortic arch aneurysm, you may be recommended the frozen elephant trunk (FET) procedure as a form of open surgery. The FET procedure is sophisticated hybrid surgery used to repair aortic aneurysms and dissections involving the aortic arch. The procedure gets its name from the appearance of the stent graft used in surgery, which is long and rigid, resembling an elephant’s trunk.
FET combines open surgery and endovascular stent grafting. During the procedure, damaged aortic tissue is replaced with a Dacron graft, and a stent graft is inserted to strengthen the aorta. This restores blood flow and reduces the need for multiple surgeries, potentially leading to faster recovery and fewer complications.

Descending thoracic aneurysm repair surgery. The damaged section of the aorta is replaced with a synthetic graft.

Aortic root aneurysm repair. If the aortic valve is damaged due to the aortic root aneurysm, it will need to be replaced with a prosthetic option. If the aortic valve is healthy, it can be spared with the David Procedure.
Locations
Discovery our cardiology experts
Meet our team of cardiologists specialising in aortic aneurysm. Whether it’s maintaining heart health or implementing innovative interventions, our experts are here to offer personalised care tailored just for you.
